cislvarese.it
LA PROVINCIA VENERDÌ 25 OTTOBRE 2013 Dichiarazione Iva standardLa Ue vuole ridurre i costiVita delle imprese più semplice con la dichiarazio-ne Iva standard con requisiti uniformi in tutta Europa. È allo studio della Ue. Potrebbe ridurre icosti per le imprese fino a 15 miliardi di euro l’anno. Cargolux: ogni sabato volo in America centraleDalle Ferrari, alle Lamborghini fino al
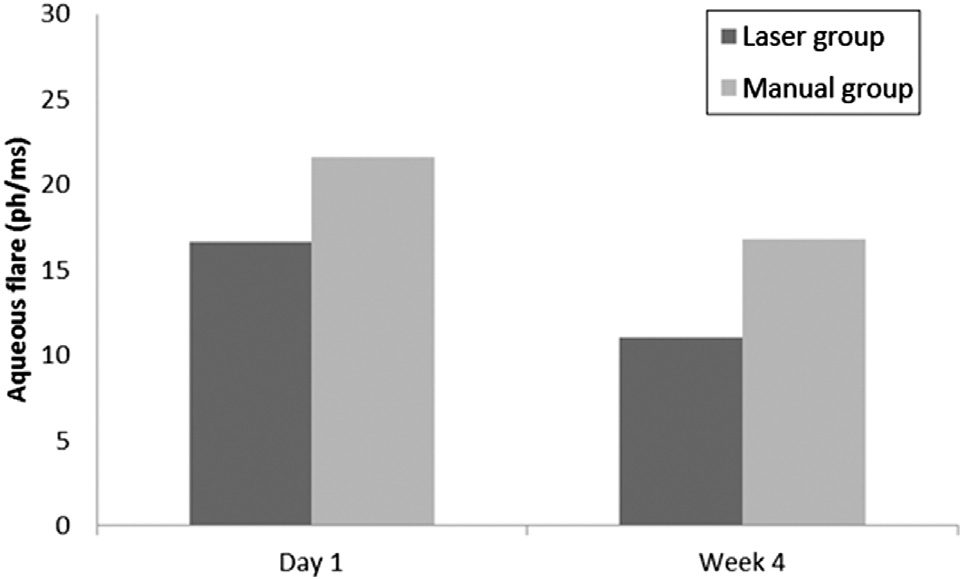 ANTERIOR CHAMBER FLARE AFTER LASER-ASSISTED CATARACT SURGERY
salt solution (BSS Plus) fluid volume used during surgery, in-terval between the laser procedure and initiation of manualsurgery steps, postoperative IOP, and the change in retinalthickness from baseline measured by OCT. Retinal thicknessmeasured by OCT included central thickness and the meanof the 4 inner pericentral and 4 outer quadrants separately,as described above, at 4 weeks. An ophthalmologist assessedpatients at 1 day and 4 weeks using slitlamp biomicroscopy(anterior segment and fundus).
ANTERIOR CHAMBER FLARE AFTER LASER-ASSISTED CATARACT SURGERY
salt solution (BSS Plus) fluid volume used during surgery, in-terval between the laser procedure and initiation of manualsurgery steps, postoperative IOP, and the change in retinalthickness from baseline measured by OCT. Retinal thicknessmeasured by OCT included central thickness and the meanof the 4 inner pericentral and 4 outer quadrants separately,as described above, at 4 weeks. An ophthalmologist assessedpatients at 1 day and 4 weeks using slitlamp biomicroscopy(anterior segment and fundus).